Healthier Lives Newsletter December 2022
14 December 2022
In this issue:
- Director’s message
- Event: Transforming Lives: 100 years of insulin
- Research results: An optimal diet for health and environment
- Podcast: Alarm bell rung on sugar
- Towards implementation: Cancer diagnostic test could be a ‘game changer’
- Challenge news: Recent visits
- New policy: MBIE announces open research policy
- In the news
- Congratulations
Director’s message
Healthier Lives research teams have been working hard in 2022 to produce research evidence that can help improve health and wellbeing in Aotearoa. Our diverse research projects have two things in common: the desire to make an immediate difference to people’s lives and a commitment to eliminating health inequities in this country. This year, we have also highlighted an issue around how research evidence is taken up and used in both policy and practice in New Zealand.

Our report on Pathways between research policy and practice raises concerns shared by many researchers that these pathways are not working effectively, and in some cases are almost non-existent. Reviving and reconstituting some of the permanent (as opposed to ad hoc) advisory structures which used to exist within the Ministry of Health would be a good way of starting to remedy this situation.
An inventory of policies relating to the major non-communicable diseases, which Healthier Lives commissioned from the Institute of Public Policy this year, reveals large policy gaps. Around a quarter of a million New Zealanders currently have diabetes and more than 20% of the population may have prediabetes. A 2021 report on the Economic and Social Cost of Type 2 Diabetes, commissioned by Healthier Lives and others, shows that these numbers will grow substantially over the next 20 years. So why doesn’t New Zealand have a national action plan to tackle diabetes? And, as a country with amongst the highest rates of obesity in the world, it’s also worth asking why we don’t have a national action plan to tackle obesity. Healthier Lives Deputy Director Cliona Ni Mhurchu recently pointed out that while we should have zero tolerance for fat shaming, obesity is a health issue that we need to address as a country.
We acknowledge that the reforms to our health system are still being bedded in. Te Pae Tata, the interim New Zealand Health Plan, contains the important goal of implementing “accessible and nationally-consistent clinical pathways” for some of the major non-communicable diseases. It also contains a new funded initiative to tackle diabetes (albeit in a single region) and a budgeted commitment for new equity-focused screening initiatives for cancer. These are valuable actions but there are no new funded initiatives for obesity or cardiovascular disease. Obesity, a major driver of other non-communicable diseases, is mentioned only once in the whole plan. As the new bodies responsible for health policy and healthcare delivery gain momentum next year, we sincerely hope to see more initiatives emerging.
We acknowledge that the reforms to our health system are still being bedded in. Te Pae Tata, the interim New Zealand Health Plan, contains the important goal of implementing “accessible and nationally-consistent clinical pathways” for some of the major non-communicable diseases. It also contains a new funded initiative to tackle diabetes (albeit in a single region) and a budgeted commitment for new equity-focused screening initiatives for cancer. These are valuable actions but there are no new funded initiatives for obesity or cardiovascular disease. Obesity, a major driver of other non-communicable diseases, is mentioned only once in the whole plan. As the new bodies responsible for health policy and healthcare delivery gain momentum next year, we sincerely hope to see more initiatives emerging.
It is important to consider both human and planetary health for our long-term well-being. A recent collaboration between the Healthier Lives and Our Land and Water national science challenges undertook a modelling “thought experiment” which showed that if our whole population adopted a healthier diet and we changed land use to produce the food for that diet, we could achieve a win-win-win for health, the environment and the economy.
The Transforming Lives: 100 years of insulin symposium, hosted by Healthier Lives and others at Parliament last month, celebrated the centenary of a life-saving medical breakthrough that transformed the treatment of type 1 diabetes. This event also showcased continuous glucose monitoring (CGM), a modern technology that can transform lives today. CGM reduces the estimated 180 extra decisions that people who are dependent on insulin must make each day just to stay healthy. It is the gold standard of care for people with type 1 diabetes, funded in Australia, Canada, the UK and much of Europe but not yet in Aotearoa. We understand that PHARMAC is currently deliberating on whether to fund CGM in New Zealand.
It’s evident that our health budget, like other areas of the economy, is under tremendous strain but the health costs of non-communicable diseases will only soar over the next two decades if we don’t act now on multiple fronts. With New Zealand’s short electoral cycle, long-term health conditions will only be prioritised if politicians know that it is an issue that their electorate cares about. That sounds like a worthy New Year’s resolution for all of us.
On behalf of Healthier Lives, I wish you and your whānau a safe, healthy and happy holiday season. Meri kirihimete me te tau hou ki a koe me tō whānau hoki.
Jim Mann
Director, Healthier Lives-He Oranga Hauora
Transforming Lives: 100 years of insulin

Healthier Lives collaborated with the Edgar Diabetes and Obesity Research Centre, Diabetes New Zealand and Lions New Zealand District 202F (Southland and Central Otago), to host the Transforming lives: 100 years of insulin symposium at Parliament House on Thursday 24 November.
This event marked a century since insulin was first used for the treatment of diabetes in New Zealand. It also highlighted continuous glucose monitoring (CGM), a technology used for the management of diabetes, which is funded in other countries but is not yet available to everyone who needs it in Aotearoa.
Transforming Lives featured researchers, clinicians, diabetes advocates and those living with type 1 diabetes, both young and old. Their presentations offered a compelling view of how far we have come in the journey to treat people living with diabetes, but also exposed how far we have to go to achieve equity of treatment in Aotearoa New Zealand.
Visit the event website to watch recordings of the presentations:
Transforming Lives: 100 years of insulin | University of Otago
Prior to the event, Healthier Lives Director Professor Jim Mann was interviewed on Breakfast TV about the need to fund new technologies. To show just how far we have come, he demonstrated some of the equipment used in the past to administer insulin.
Improving the lives of Kiwis living with diabetes | Breakfast (on Facebook)
A recent article in The Conversation delves into the history of diabetes treatment and asks why we are not funding the latest life-changing technology for those living with diabetes.
100 years after insulin was first used, why isn’t New Zealand funding the latest life-changing diabetes technology? | The Conversation
An optimal diet for health and the environment
The diet our population eats has a major impact on both human and planetary health.

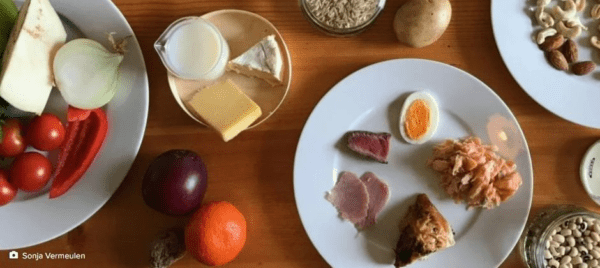
Healthier Lives research, led by Dr Cristina Cleghorn at the University of Otago Wellington, has identified an “optimal diet” for New Zealand which contains all the nutrients recommended for health, is relatively affordable, and produces greenhouse gas emissions levels at levels that don’t exceed “planetary boundaries”, i.e. environmental limits within which humanity can safely operate.
This optimal diet includes fruits, vegetables, dairy, legumes, wholegrains and some fish, but very little beef, lamb, pork and poultry. Dr Cleghorn modelled what the effects on health and health costs would be if this diet was adopted nationally. The project’s recently published findings show that there would be significant health gains (approximately 1.4 million Quality Adjusted Life Years), cost savings to the health system ($19.7 billion in 2011 value) and reductions in health inequity between Māori and non-Māori.
However, most people don’t eat such a diet and it would be unrealistic to expect everyone to adopt it overnight. The research team is therefore investigating strategies that could help us, as a whole population, move towards a healthier diet in the future.
Parallel research led by Dr Andrew Reynolds in collaboration with Dr Cleghorn and Professor Cliona Ni Mhurchu has examined different ways of replacing red and processed meat in the New Zealand diet. Their findings, due to be published soon, indicate that a range of meat replacement options would improve health, equity, health systems costs and greenhouse gas outcomes (although the cost to individuals varies between the different options). There will be more on this to come in future newsletters.
Growing for good: A ‘win-win-win’ plan for future food production

In related research, Dr Cleghorn teamed up with researchers from Our Land and Water National Science Challenge to model what the effects would be if we changed the current use of land in New Zealand to grow the food needed for a version of the optimal diet that was adjusted to include some beef and lamb and a little more dairy.
The results of this “modelling exercise and thought experiment” have recently been published. Professor Richard McDowell, lead author and chief scientist for the Our Land and Water National Science Challenge, says: “[t]he key take-out is that it is possible to strategically redesign future food production in New Zealand in a way that has significant co-benefits for our people and our environment.”
Read the paper about the optimal diet:
Cleghorn C, Nghiem N, Ni Mhurchu C. Assessing the Health and Environmental Benefits of a New Zealand Diet Optimised for Health and Climate Protection. Sustainability. 2022; 14(21):13900.
Read the paper about changing land use:
Growing for Good: A ‘Win-Win-Win’ Plan for Future Food Production | Healthier Lives
Listen to Professor Richard McDowell (Our Land and Water) discuss the findings about land use in an interview with the National Business Review Online:
Changing what we grow and where could give Kiwis a healthier diet | YouTube
Alarm bell rung on sugar


Professor Cliona Ni Mhurchu, Healthier Lives deputy director, and Dr Helen Eyles, Healthier Lives researcher (both of the University of Auckland) are among the experts featured in Sweet As, a podcast from True Story which investigates sugar and its connection to the obesity epidemic.
It’s a fascinating episode, which races through the history of sugar consumption from pre-history to the post-war rise of convenience foods. Along the way it covers topics such as the use of sugar to treat newborn babies who have low blood glucose, an intriguing experiment about consuming ultra-processed foods, and the links between sugar and increasing levels of blindness in the Pacific.

Cliona and Helen discuss various strategies for tackling the obesity epidemic, some which definitely don’t work and some which just might, and conclude that there is a lot more we could do to make a difference. Even if you think you know a lot about sugar, this 44-minute podcast might surprise you.
‘Fat-shaming doesn’t work’ says nutritionist, who wants urgent political action | Stuff.co.nz
Cancer diagnostic test could be a ‘game changer’
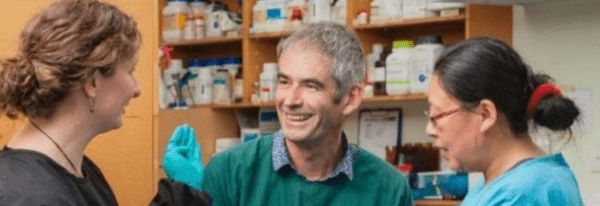
Advocate and founder of the Southland Charity Hospital, Melissa Vining, aims to raise $1 million to carry out clinical trials on an affordable diagnostic test for bowel cancer that has been developed through Healthier Lives research.
The test works by detecting circulating tumour DNA in the bloodstream. Among many other potential uses, it could be used to confirm the likelihood of bowel cancer prior to a colonoscopy, which would help to reduce colonoscopy waiting lists.
The test is conducted via a simple blood sample and handheld testing device, which makes the technology highly portable. That is good news for people living in rural communities. Healthier Lives principal investigator Professor Parry Guilford (pictured above) leads a team at the University of Otago which has been developing the test over the past six years, alongside Professor Cristin Print and his team at the University of Auckland.
It is exciting to see this Healthier Lives research getting closer to implementation where it can make a real difference for cancer patients.
Bowel cancer blood test could be a ‘game changer,’ Vining says | Stuff.co.nz

Jordon Lima is currently undertaking her PhD as part of the Healthier Lives ctDNA project. The University of Otago recently featured an interview with Jordon on its online bulletin board where she discusses her dual interests in undertaking biomedical research and learning te reo Māori.
PhD candidate Jordon Lima on reclaiming te reo Māori | University of Otago
Recent visits
Two recent visits have encouraged and supported the work of Healthier Lives researchers.
In October, distinguished US researcher and chair of the Healthier Lives International Science Advisory Panel (ISAP), Professor Shiriki Kumanyika, visited Aotearoa to undertake a formative review of five Healthier Lives research projects. The opportunity for our research teams to engage with her about their work was an enjoyable and greatly appreciated experience.
Following these review meetings, Professor Kumanyika travelled to Melbourne to receive the World Obesity Federation William Philip T James Award for outstanding achievement in the fields of obesity surveillance, prevention, and management, an award she shared with Professor Boyd Swinburn from the University of Auckland.
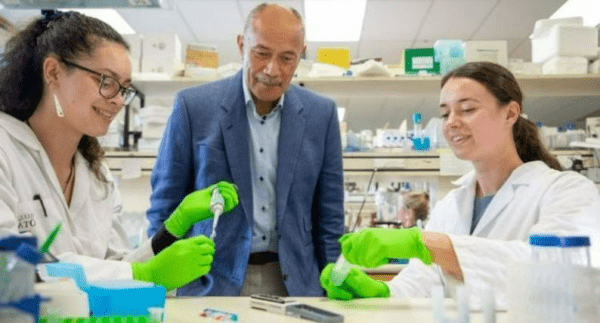
In November, the chair of the Healthier Lives Governance Group and Kāhui Māori, Sir Jerry Mateparae, spent the day in Ōtepoti talking to investigators and doctoral students about their research and its potential applications. This included a project which aims to make the design of health interventions more equitable, a new study that is the first New Zealand trial of international research that has achieved remission of diabetes, and epigenetic research that is incorporating a Te Ao Māori lens. Sir Jerry also visited the Guilford laboratory where PhD students Jordon Lima and Alice McAtamney explained how ctDNA research can aid early cancer detection.
MBIE announces open research policy
MBIE recently announced a new policy to increase equity of access to peer-reviewed research outputs and increase the potential impact of research. From 1 January 2023, all new research funded by MBIE must publish peer-reviewed journal articles and conference proceedings through open access pathways.
Open research policy | MBIE
In the news
Sue Crengle, a ‘force of nature’

Professor Sue Crengle (University of Otago and Te Aka Whai Ora), Healthier Lives principal investigator, featured in a NZ Doctor profile about her journey from GP-in-training to specialist GP, researcher, and now board member of Te Aka Whai Ora.
Sue leads Healthier Lives’ Systems change for health equity project which is creating and testing tools to ensure that the design and implementation of new health interventions will achieve equitable outcomes.
Sue Crengle: Calling to account | NZ Doctor
Indigenous workforce critical to equity

Taria Tane (University of Auckland), Healthier Lives doctoral candidate, spoke at the National Rural Health Conference in Christchurch about her research as part of Healthier Lives’ Manawataki Fatu Fatu for ACCESS project.
When reviewing the academic literature on cardiovascular services for rural Indigenous communities, she was only able to find one publication from New Zealand.
Taria plans to improve this situation with her own research focusing on understanding the barriers and facilitators to quality cardiovascular care for rural Māori.
Lack of rural Māori services data raises hackles | NZ Doctor [Subscriber access]
The benefits of lower speed limits
Professor Simon Kingham (University of Canterbury), Healthier Lives co-principal investigator, discussed the benefits of lower speed limits in our towns and cities. Not only would lower speed limits reduce road deaths and injuries, but they would also reduce pollution, noise, and health inequalities, as Māori, younger people and low-income communities are over-represented in road injury and death.
Lower speed limits don’t just save lives – they make NZ towns and cities better places to live | The Conversation
Census failings raise question of democratic representation

Andrew Sporle, Healthier Lives deputy director, commented on findings that the 2013 census undercounted Māori by almost 50,000, and the implications that this has for our democracy. The Data Iwi Leaders’ Group claimed that the undercount “brings into sharp focus the importance of quality data, and the disproportionate impact on Māori when it is not done correctly”.
The ‘big maybe’ over Māori seats in Parliament due to census undercount | Radio NZ
Dr Rawiri Mckree Jansen joins Te Aka Whai Ora
In August, Healthier Lives kaupapa partner Dr Rawiri McKree Jansen joined Te Aka Whai Ora, The Māori Health Authority, as chief medical officer.
Dr Rawiri Jansen | New Chief Medical Officer for Te Aka Whai Ora – The Māori Health Authority | Waatea News [6m 52s]
25 years on from life-saving discovery

Stomach cancer is more common among Māori and Pasifika and one of the reasons for this is inherited alterations in a gene called CDH1. This year marks 25 years since the discovery of these genetic changes by Healthier Lives deputy director Professor Parry Guilford (University of Otago).
How a medical breakthrough has saved the lives of many New Zealanders | Newshub
Warm congratulations to…

Dr Sandra Hanchard (University of Auckland), Healthier Lives researcher, who received the inaugural Pacific Research Fellowship, jointly funded by the Heart Foundation and Pūtahi Manawa (Healthy Hearts for Aotearoa New Zealand).
Inaugural Pacific Research Fellow aims to enhance equity in discharge planning | NZ Doctor

Dr Andrew Reynolds (University of Otago), Healthier Lives principal investigator, who was awarded a Heart Foundation Senior Fellowship.
Heart Foundation 2022 research grants announced | Heart Foundation

Dr Cristina Cleghorn (University of Otago Wellington), Healthier Lives principal investigator, who was awarded a Sir Charles Hercus Fellowship from the Health Research Council of New Zealand.
Links between active travel and health to be studied as part of $11.1M awarded to NZ researchers | Health Research Council

Associate Professor Dianne Sika-Paotonu (University of Otago Wellington), Healthier Lives co-principal investigator and science leadership team member, who was has been elected to chair the Health Research Council’s Pacific Health Research Committee.