Improving life and outcomes for cancer patients
22 November 2017
Having treatment for cancer is a traumatic experience for anyone. But scientists are working towards making it easier, and more effective.
Most of us will be affected by cancer in some way during our lifetimes; so we know that cancer treatments are invasive, often painful, and often come with a raft of unpleasant side effects. What’s more, patients usually don’t know if the drugs are working until they’ve had several taxing cycles of treatment.
Research being undertaken by Healthier Lives scientists is looking to take some of the stress and pain out of cancer treatment, by developing a way to make it easier for doctors and patients to understand how treatment is working, far sooner, and without the need for invasive and expensive scans.
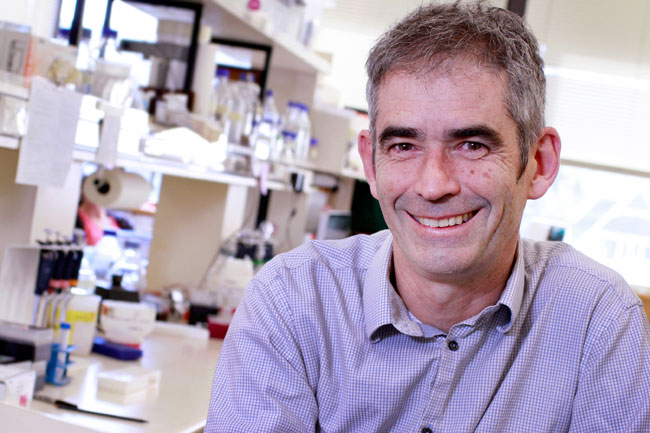
A team led by Otago University’s Professor Parry Guilford is working on a project as part of the Healthier Lives National Science Challenge to develop minimally invasive markers for cancer detection.
In practice, that would mean instead of months of chemotherapy and undergoing a CT scan in a hospital to see if the treatment has worked, a patient could have a simple blood test at their local clinic after a week or two which would give doctors the same information. Treatment options could then be adjusted accordingly. It could also be used to check on cancer progression and relapse.
Measuring markers in the blood

The technology works by measuring biomarkers of cancer in the blood – in this case, what’s known as circulating tumour DNA (ctDNA).
Professor Guilford explains: “Every tissue in the body – even cancers – have cells which die every few days. There’s always a turnover of cells. When those cells die, their DNA gets spilled into the bloodstream.
“You can recognise the DNA which has come from the tumour through the presence of mutations in the DNA sequence. So…by using DNA sequencing techniques you can identify genes involved in cancer behaviour, and you can find mutations in those genes. By quantifying the number of mutated DNA molecules in the blood stream you effectively have a measure – or a marker – of the size of a cancer… if the levels fall away, the tumour is getting smaller.”
Improving treatment while saving time
The applications for this are wide-ranging, and hugely beneficial for both patients and clinicians, saving time and improving treatment.
“At the moment if you were to begin chemotherapy you would have that treatment for say six or so cycles – two or three months”, says Professor Guilford. “Then you’d have to have a CT scan and there’d be some kind of decision made on whether the treatment was effective or not. Quite often it’s not effective, so you’ve gone through all that misery of the toxic chemotherapy and achieved no clinical benefit.
Early stage treatment indicators
“The technology is very useful to indicate at an early stage whether a patient is responding to treatment, so within a week or two of starting treatment we could make an early call on whether it is useful or futile. If it’s useful you carry on, if not, you can swap it out. It means that clinicians can become much more nimble in how they treat patients.”
For patients it means fewer potentially harmful side-effects, fewer visits to hospital for invasive and time-consuming tests and ultimately more effective cancer treatment.
Early success with colorectal cancer
In their study so far, Professor Guilford’s team has identified changes in patients with colorectal cancer within days of starting treatment. “If the treatment is working well, levels [of ctDNA] fall through the floor within a few days”, he says.
Equally, if levels are not dropping: “you’ve got reason to worry that the whole treatment is not working, and therefore the oncologist will think about changing the medication pretty quickly.”
Potential in melanoma treatment

In another part of the project, led by Auckland University’s Professor Cristin Print, genomic blood tests are also being used; this time to detect melanoma tumour relapse in patients after treatment.
“We are focussed on identifying relapse early,” says Professor Print.
“This means hopefully patients can survive a relapse by getting earlier treatment; we can catch a relapsing tumour before it becomes un-treatable or spreads further.”
The other benefit to patients is less invasive and more regular monitoring.
Reducing inequities
The benefits also extend to improving the whole health system when it comes to cancer management. That means reducing inequities in the health system by improving access to care for vulnerable and remote communities. Patients who might find it difficult to go to a big ‘hospital on a hill’ can have marae-based or community-based care.
And costs come down for District Health Boards, with less need for scanning. “Patients should receive better care at lower cost,” says Professor Guilford. “It’s the sweet spot for DHBs.”
The technology is already starting to be used overseas. In their three year Healthier Lives project, Professor Guilford’s team is adapting it to local New Zealand conditions, for example allowing for distance and time difficulties when working with patients in remote areas in the country, and making sure the technology is affordable to the New Zealand health system.
Expanding to include other cancers
As well as Professor Guilford’s team focussing on colorectal cancer and Professor Print’s work on melanoma, the researchers are expanding the ctDNA marker research to cover breast, stomach and childhood cancers too, through additional funding.
The next stage will be to develop the practical details of getting the research out of the lab and into the community.
That will mean finding a diagnostic laboratory, and getting efficient and timely processes in place to make the technology work within the health system. It’s a change from the usual way University researchers work.
Making a difference, meeting the challenge
“All those details which you don’t normally worry about in a research lab, are things we need to think about as part of the National Science Challenges”, says Professor Guilford.
“That’s the feature of these Challenges, particularly Healthier Lives. It’s not just about doing the research; it’s about making a difference at the end of it.”
Professor Guilford says this practical research will result in a change to cancer management. “In five years’ time, this will be routine clinical practice in New Zealand.”
“It’s quite advanced technology. We’re not in dreamland about ‘one day this might work’. It’s going to work. Our job is to get it implemented into the health care practices in the country. It’s not one where we say, maybe in 10 years we might have some clinical trials. This is happening now – we have to keep on going and we’ll get there.”
Science leader and principal investigator ctDNA project:
- Professor Parry Guilford, University of Otago
Co-principal investigators:
- Dr Chris Jackson, University of Otago
- Professor Cristin Print, University of Auckland