HE AHA TĀ MĀTOU I TŪHURA AI
What we investigated
Co-funding
NGA PUTANGA ME TE PĀNGA
Outcomes and Impact
WHAKAWHITI MŌHIOTANGA
Knowledge Exchange
BetaMe
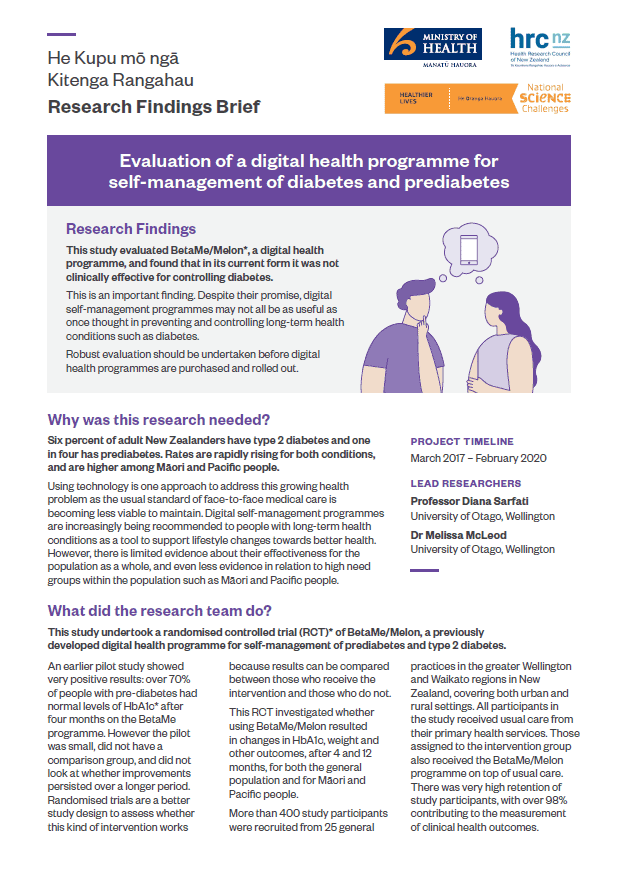
Research Findings Brief
This study evaluated BetaMe/Melon, a digital health programme, and found that in its current form it was not clinically effective for controlling diabetes.
This is an important finding. Despite their promise, digital self-management programmes may not all be as useful as once thought in preventing and controlling long-term health conditions such as diabetes.
Robust evaluation should be undertaken before digital health programmes are purchased and rolled out.