HE AHA TĀ MĀTOU I TŪHURA AI
What we investigated
Take | Issue
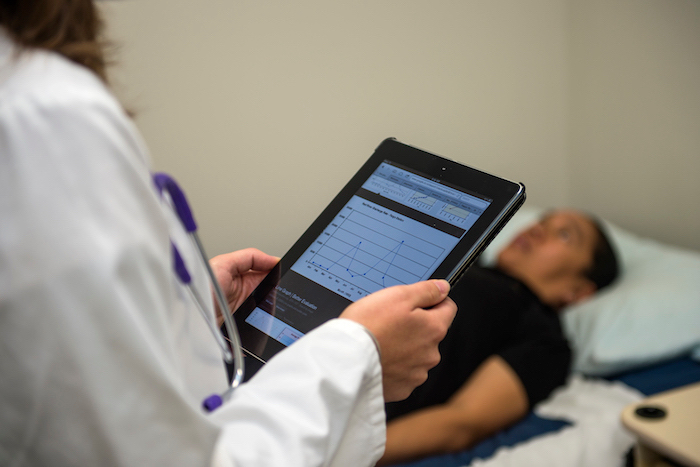
There are significant ethnic and social disparities in the prevalence and outcomes of type 2 diabetes in Aotearoa New Zealand, resulting from a range of complex factors such as wider social determinants of health, levels of engagement with the health system and management of the condition and its complications.
Whāinga | Aim
Mana Tū is a co-designed programme which deploys skilled and supported Kaimanaaki-whānau to help people with poorly controlled diabetes manage their own health. The Kaimanaaki work with General Practice (GP) teams while being supported by a central hub, which co-ordinates a range of support systems.
This project investigated whether Mana Tū can improve health behaviours and outcomes for people with poorly controlled diabetes and whānau living with pre-diabetes.
Huarahi I Whāia | Approach
Mana Tū is a co-designed programme which deploys skilled and supported Kaimanaaki-whānau to help people with poorly controlled diabetes manage their own health. The Kaimanaaki work with General Practice (GP) teams while being supported by a central hub, which co-ordinates a range of support systems.
This project investigated whether Mana Tū can improve health behaviours and outcomes for people with poorly controlled diabetes and whānau living with pre-diabetes.
Co-funding
This project was funded by:
The Ministry of Health, Health Research Council of New Zealand, and Healthier Lives National Science Challenge, as part of the Long-Term Conditions Partnership.
NGA PUTANGA ME TE PĀNGA
Outcomes and Impact
Putanga | Outcome
The trial demonstrated significant improvements in five of six ‘domains of change’ that are closely related to effective chronic disease management: nutrition; self-management; physical; health literacy; cultural safety; and smoking. Only the last of these showed no change.
One of the biggest changes was an increase in the amount of fruit and vegetables consumed daily by Mana Tū participants. They also increased their level of physical activity by 10% on average. By far the biggest increase was in their sense of cultural safety and readiness to engage with health and social services, which rose by 84%.
Over two thirds of the intervention group had some reduction in HbA1c over the twelve-month period but the difference between the intervention and control groups was not statistically significant. There was little change in blood pressure, low density lipoprotein (LDL) or high density lipoprotein (HDL) and no difference between the intervention and control groups. The observed change in HbA1c was comparable to changes found in systematic reviews of chronic disease management programmes.
The evaluation found that the Mana Tū programme had a positive impact on the lives of participants. Importantly, there was a clear improvement over time in their confidence to achieve goals and in feeling empowered to do the work needed to achieve future goals.
Te Ara Kei Mua | Next Steps
Many communities around New Zealand would benefit from wider roll out of a case management programme addressing the social determinants of health.
WHAKAWHITI MŌHIOTANGA
Knowledge Exchange
Puka Rangahau | Academic Publications
-
-
- Tangata Hourua: A framework drawing from Kaupapa Māori and Pacific research methodologies AlterNative: An International Journal of Indigenous Peoples (2022)
- Understanding the workforce that supports Māori and Pacific peoples with type 2 diabetes to achieve better health outcomes. BMC Health Serv Res 22,672 (2022)
- Māori and Pacific peoples’ experiences of a Māori-led diabetes programme New Zealand Medical Journal (2021), 134:1543
- Mana Tū: a whānau ora approach to type 2 diabetes. The New Zealand Medical Journal (2018), 131:1485
- Indigenous health worker support for patients with poorly controlled type 2 diabetes: study protocol for a cluster randomised controlled trial of the Mana Tū programme. BMJ Open (2018), 8(12), e019572
-
Pāpāho | Media
-
-
- Research shows navigators effective for Maori health Waatea News (2020)
- More Māori and Pacific health workers should be doctors, nurses and managers – Dr Matire Harwood Stuff.co.nz (2019)
- Mana Tū Diabetes NZ (2019)
- Maori approach to diabetes treatment studied Waatea News (2017)
-
Kōnae Whakaata | Video
-
-
- What is Mana Tū – Taria Tane | LTC Forum 2020 YouTube, July 2020
-