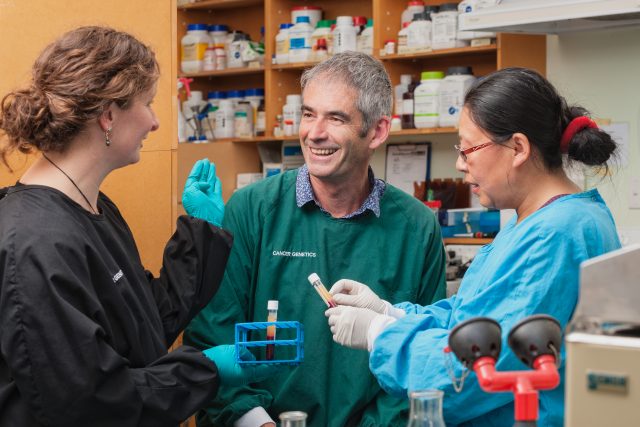
Cancer project takes aim at healthcare inequities
26 April 2018
The Healthier Lives project ctDNA for better cancer management has recently been highlighted in the media for its potential to reduce healthcare inequities for Māori and people living in rural communities.
The research team, led by Professor Parry Guilford, is working on a blood test that detects circulating DNA (ctDNA) in the bloodstream of cancer patients. CtDNA is cancer-derived DNA that leaks out from tumours into the blood stream.
The researchers now have a working innovative ctDNA test which is successfully tracking disease burden in many colorectal cancer and melanoma patients.
Because the incidence of colorectal cancer and melanoma in New Zealand is among the highest in the world, the researchers are starting with these two cancers but the method can be applied to other cancers. This test has the potential to become standard of care in New Zealand for most cancers, and will lead to major changes in the management of cancer patients and will reduce health care inequities.
Principal investigator Professor Parry Guilford, University of Otago, says the test provides a useful measure of whether or not a tumour is growing or shrinking, and therefore provides information on whether or not any particular treatment is working.
“In addition, if someone has finished treatment, it will be possible to keep an eye on them and see if it’s coming back”, he says.
This simple blood test could help reduce health inequities for Māori and other cancer patients in isolated parts of the country because it makes the testing much more straightforward and accessible for everyone.
Currently, patients have had to go into hospital for scans and X-rays, and these have a number of limitations. The current technology is also expensive, there’s a significant queue, and because of the radiation, you can only get them every eight to ten weeks, explains Professor Guilford. The scans are also only available at New Zealand’s larger hospitals, which makes it tougher for Māori and others who live in rural or isolated parts of the country.
The DNA blood sampling method is beginning to be used by researchers and clinicians internationally, and could in principle be applied to monitor every form of cancer (with the possible exception of brain cancer) because they all release DNA into the blood stream.
Professor Guilford, Professor Mike Eccles and Professor Cris Print, University of Auckland, have been working to adapt the technology to New Zealand conditions. This has involved identifying a method that stabilises blood samples for up to two weeks at room temperature, allowing for long lag times in getting samples to the testing laboratory. They have also developed a multiplex method which will significantly reduce the cost to make it accessible for all patients. In addition, they have begun development of a medical device which will be used to dramatically increase test sensitivity, opening up the possibility of using ctDNA for early diagnosis.
Planned future clinical studies include trials involving Māori and non-Māori patients living in rural communities who are under surveillance for cancer recurrence.
“Whether it be rural GPs or clinics on marae, this has a real potential to take this surveillance of patients in treatment away from hospitals and out to the communities.”
Related news
New monitoring method could help Māori cancer patients University of Otago
Blood test trials aim to reduce higher Māori cancer rates RadioNZ
‘Critical’ test could help Maori cancer patients Otago Daily Times
Blood test checks cancer cures Waatea News
Read more about the ctDNA for better cancer management project
Improving life and outcomes for cancer patients
CtDNA for better cancer management: the application of precision oncology to the New Zealand healthcare system research page