Healthier Lives Kōrero Tahi 2024 – presentations
18 March 2024
Healthier Lives Kōrero Tahi 2024 – equity and beyond
13-14 February, Te Papa Tongarewa, Wellington
More than 200 kaupapa partners, stakeholders and researchers gathered at Te Papa Tongarewa and online for Kōrero Tahi 2024 where research findings from the second phase of Healthier Lives were presented.
This newsletter provides a taste of the rich kōrero and links to recordings of the presentations in the following sessions:
- Opening remarks by Sir Jerry Mateparae
- Keynote address by Professor Nick Wareham
- Keynote address by Max Rashbrooke
- Healthy food and physical activity environments
- Culturally-engaged healthcare for Māori and Pacific peoples
- Precision medicine
- Report launch: Co-designing health research in Aotearoa New Zealand
All photos by Luke Pilkinton-Ching (visionphotography.co.nz)
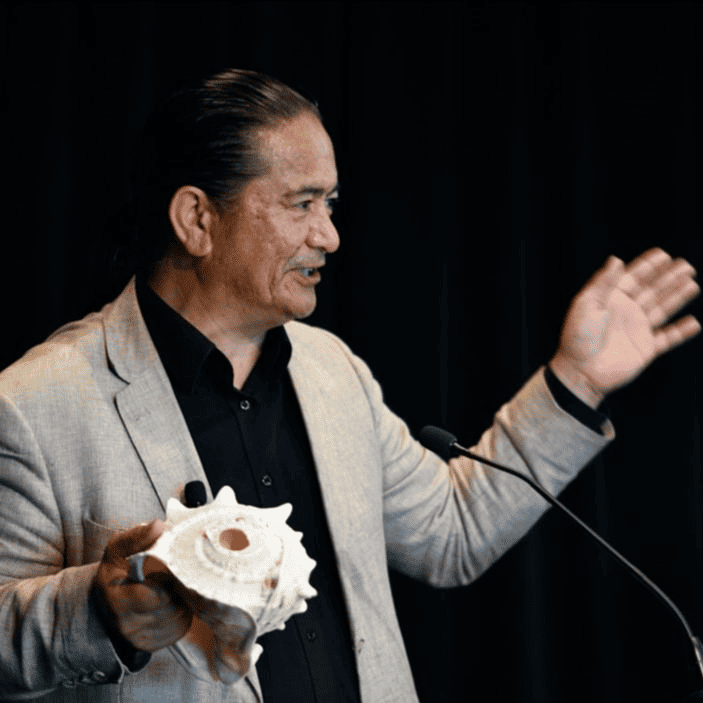
Opening remarks by Sir Jerry Mateparae
Sir Jerry Mateparae, Chair of the Healthier Lives Governance Group and Kāhui Māori, opened Kōrero Tahi 2024: equity and beyond. He described the defining features of Healthier Lives: co-governance, co-designing research with communities, and clear pathways to implementation, which was facilitated by Challenge support for researchers throughout their projects.
Opening remarks – Sir Jerry Mateparae [5 min]
Keynote address by Professor Nick Wareham
Professor Nick Wareham (University of Cambridge) is a member of Healthier Lives’ International Science Advisory Panel.

Nick Wareham spoke about type 2 diabetes as a major public health issue, driven by a wider societal problem. He suggested that it is often impossible to obtain definitive evidence before addressing public health issues – instead, governments need to take bold and decisive policy action, based on the best available observational data, and then evaluate the impact of that action. One example of bold policy action is the UK Government’s introduction of a levy on sugar sweetened beverages in 2018. Six years on, there are signs that the levy is working.
Preventing type 2 diabetes: going upstream – Professor Nick Wareham [60 min]
Keynote address by Max Rashbrooke
Max Rashbrooke is a New Zealand writer and public intellectual, with twin interests in economic inequality and democratic renewal.
Max Rashbrooke began his talk on the economic drivers of ill health with a quote from the Robert Wood Johnson Foundation: “Health starts where we live, learn, work and play”. Economic inequality in Aotearoa New Zealand affects all these domains, for example 30-50% of our rental houses are substandard and four in ten of the children living in poverty have a parent working full time. Shifting from an extractive economy to an inclusion economy which invests in people and infrastructure would help to reduce the underlying causes of health inequities.
Where health starts: tackling the economic drivers of illness – Max Rashbrooke [36 min]
Healthy food and physical activity environments
Healthy food environments

Rising rates of non-communicable diseases are a direct result of what we eat, according to session co-chair Michelle Mako (Manatū Hauora). She argued that we need to think more broadly about the factors driving poor diet and strengthen our local food supply.
Professor Cliona Ni Mhurchu (University of Auckland) talked about what she has learned from evaluating the National Healthy Food and Drink Policy. “A policy alone is not going to do anything, it’s a piece of paper”, she said. Successful policy implementation needs strong leadership, resources to support its implementation in the real world, and regular monitoring and feedback loops.
Magda Rosin’s PhD has focused on putting together the pieces of the puzzle that could support the implementation of the National Healthy Food and Drink Policy. An online, searchable product database to help food retailers classify foods against Policy criteria was identified as the single most-needed tool, so researchers teamed up with a product designer to create a prototype of the Healthy Kai Checker. Moving our population towards healthier and more sustainable kai would have health and climate co-benefits.
Dr Cristina Cleghorn (University of Otago) reported on consultation with policymakers and communities which identified more than a hundred potential policies that, if introduced, could support this shift. Narrowing this list to five stakeholder-selected and evidence-based policies, she has modelled their impact on health.
Dr Hemi Enright has been exploring Māori views of healthy and sustainable kai as part of his training in public health. The ongoing process of colonisation has severely impacted the ability of Māori to enact kaitiakitanga over natural resources and whenua, he said. The right of Māori to enact “Kai Rangatiritanga” needs to be recognized as part of moving towards healthier and more sustainable kai in Aotearoa.
Towards a healthy sustainable food system for Aotearoa [53 min]
Healthy physical activity environments
Session co-chair Kathryn King (Waka Kotahi) argued that using active forms of transport is one of the easiest ways for people to build physical activity into their daily lives. While “New Zealanders are amongst the most car-dependent people on our planet” it doesn’t have to be that way, she said. Other countries have turned around their car-dependent transport systems.
E-bikes have huge potential for increasing physical activity, reducing greenhouse gas emissions, and reducing household fuel costs but as Professor Karen Witten (Massey University) noted, they are ubiquitous in some communities and absent in others. She spoke about three e-bike trials in Māngere – a community where e-bikes were mostly absent. Conducted in partnership with community organisation Triple Teez, the trials have been enthusiastically received by community members.

We live and work in and around Māori and non-Māori environments. Dr Kimiora Raerino (Massey University) asked mana whenua how they see themselves represented in the Māngere environment. The cultural features of streetscapes and community spaces can create a sense of belonging and pride, but more work is needed to reimagine public spaces because elements important to Māori are not currently seen and uplifted enough in these spaces.
Professor Simon Kingham (University of Canterbury) described research investigating the best way to make shared transport options available within residential communities, which he believes has never been done before in Aotearoa New Zealand. There can be tensions when you ask people to share things, he noted, but there are benefits too – improved accessibility, better mental health, and greater community cohesion.
Els Russell unpacked the findings from her Master’s research project which examined Māori residents’ experience of social housing. She found that wellbeing in social housing is influenced by several factors, including complex negotiations with the social welfare system, the extent to which Māori can establish a sense of belonging in these spaces, and their ability to access the people and places that are important to them in the wider environment.
The ability of active, shared and low carbon transport interventions to enhance wellbeing [55 min]
Culturally-engaged healthcare for Māori and Pacific peoples
Heathier Lives Deputy Director Andrew Sporle (iNZight Analytics) introduced day two by asking “how do you create sustainable change on a budget?” He outlined Healthier Lives’ approach to commissioning high quality, mission-led research, capable of “changing practice, expectations, and generations”.
Culturally engaged healthcare overview [6 min]
The culturally-engaged healthcare session was led by co-chairs Megan Tunks (National Public Health Service) and Dr Viliami Puloka (Health Promotion Forum). Dr Puloka explained that time is more than what is on the clock. It’s “the willingness to give of yourself”, he said. We often engage by default, and far too often Māori and Pacific people feel that they are just an appendage to research processes. Engagement with Māori and Pacific people must be by design, not default.
Community-led research for sustainable futures
Associate Professor Riz Firestone (Massey University) introduced her team’s “malaga of learning” (learning journey) through Oire Tokoroa, a family-centred health programme co-designed with South Waikato Pacific Islands Community Services. “Families are the building blocks of society”, she said. “We wanted to learn about how to engage and work with groups of families”.
Penina Hitti (Massey University) spoke about researchers bringing integrity and humility to the co-design relationship. “We want to know if you care about us”, the leader of the community partner organisation told her. Through listening to the stories of family members, the researchers learned about the not-so-obvious causes of health problems, and the complex role that food plays in families.

Elizabeth Okiakama (South Waikato Pacific Islands Community Services) worked with vaevae orooro (family champions) through ongoing talanoa (conversations). The vaevae orooro created the Kai Tari Cookbook, featuring healthy recipes with Pacific flavours. They were the champions in making the change for themselves and their families, she said, “and they continue to make healthy choices today”.
Community-led research for sustainable futures [22 min]
A DiRECT approach to weight loss in Aotearoa

Dr Andrew Reynolds (University of Otago) discussed the promising early results of the Te Kaika DiRECT study, which is testing the acceptability and efficacy of a weight loss programme for the remission of type 2 diabetes. The impetus for this trial came from patients at Te Kaika Hauora, a Māori health provider in South Dunedin, who approached the medical director because they weren’t happy with the options available to help them lose weight.
Kate Campbell, a doctoral student working on the project, introduced her qualitative research with participants in the study. Her findings showed that dietitian support was crucial for the success of the programme. With this support, the control group also achieved weight loss although not to the same extent as participants in the main intervention.
Associate Professor Justine Camp (University of Otago) talked about the next steps for this research, including expanding to a nationwide trial and comparing outcomes with GLP-1-RA (glucagon-like peptide-1 receptor agonists) medication. The team’s underpinning Kaupapa is that what is good for Māori is good for all and they want to contribute to mauri ora.
A DiRECT approach to weight loss in Aotearoa [22 min]
Partnering with Māori and Pacific community providers to support effective implementation of health programmes and services
The Healthier Lives Implementation Network has been established to support community-based health providers interested in implementing programmes that have been shown to improve health and wellbeing. Akarere Henry, Renei Ngawati and Sulita Povaru-Bourne described how programmes developed through Healthier Lives research are already being adapted and piloted by new communities, facilitated by the Network.
Healthier Lives Implementation Network [30 min]

Front: Darrio Penetito-Hemara, Akarere Henry, Renei Ngawati, Dianne Sika Paotonu

Session co-chair Selah Hart (Te Aka Whai Ora) spoke about the importance of health equity and the role research plays in informing decisions about healthcare practices and policies. Research should be accessible to Māori and Pacific communities and curated from their lens, she said. Introducing two research programmes that are tackling systemic aspects of health inequity, session co-chair Markerita Poutasi (Te Whatu Ora) spoke about how the health system can learn from communities as well as from research outcomes.
Implementing equitable health interventions – tools for use in the Aotearoa New Zealand context
Dr Karen Bartholomew (Te Whatu Ora) outlined the implementation science research led by Professor Sue Crengle which is focused on reducing the ongoing ethnic-specific health inequities that persist, even when other factors are accounted for. At the current rate, it will take 75 years to eliminate the life expectancy gap between Māori and non-Māori. The research aims to help the mainstream health system accelerate towards that goal.

Michelle Lambert (University of Otago) described the tools which have been created to support equitable implementation in the mainstream health system, including: an equity-focussed “process” framework to guide the planning, design, monitoring and evaluation of new health programmes; and a tool to help teams assess their “equity readiness” to implement a new intervention and generate an action plan.
Implementing equitable health interventions [36 min]
Designing heart health services to achieve Māori and Pacific health equity
Dr Corina Grey (Ministry for Pacific Peoples) described the health system access gaps that exist at many points along the journey of Māori and Pacific patients who need care following cardiac events. She outlined plans to produce an equity roadmap towards eliminating these.

Workforce development is key to addressing health inequities and the Manawataki Fatu Fatu project (co-funded by Healthier Lives and the Heart Foundation) has had a significant focus on supporting the next generation of Māori and Pacific researchers. Team members Dr Karen Brewer, Dr Sandra Hanchard, Tāria Tane, Rochelle Ellison-Lupena, and Dr Tua Taueetia-Su’a spoke about the highlights and challenges of their own research projects.
Designing heart health services to achieve Māori and Pacific health equity [53 min]
Precision medicine
Precision medicine has potential to improve how we screen, diagnose, and treat life-threatening diseases, as outlined by session co-chair Dr Sayali Pendharkar (Manatū Hauora). A long-term insights briefing paper, published by the Ministry last year, is a first step towards developing a cohesive national strategy for precision health.
Precision medicine for cancer
Circulating tumour DNA (ctDNA) can be used as a precision medicine tool for monitoring cancer treatment. According to Professor Parry Guilford (University of Otago) it could reduce reliance on large hospitals and lead to better cancer care, especially for people living in rural communities. It gives clinicians information about how a patient is responding to cancer treatment in close-to-real time, enabling them to rapidly identify when a treatment is not working and switch to another treatment, and it can also help patients understand how things are going for them.

PhD student Jordan Lima talked about her “Kaupapa Ngāti Porou” research: “I’m working with my communities…to figure out how ctDNA would work for us”, she said. If we introduce ctDNA as a cancer diagnostic test, we will be diagnosing a lot more cancers and this brings the fear of “the C word” so we need to communicate that cancer is treatable, and more treatable when diagnosed early.
Dr Sandra Fitzgerald (University of Auckland) described several applications of ctDNA currently in the research pipeline. One of these is developing an affordable test for use in Aotearoa New Zealand that can replace the need for a biopsy to identify specific mutations, enabling patients to receive low-toxicity, targeted treatment which can give them a quality of life they wouldn’t have with chemotherapy.
Professor Cris Print (University of Auckland) is often asked whether introducing ctDNA to monitor cancer could save money for the health system. He presented data from overseas showing that ctDNA technologies improve cancer care and are likely to be cost neutral. The bottom line is that “more patients receive the right treatment for the same cost.”
Improving cancer diagnosis and treatment with ctDNA [53 min]
Precision medicine for cardiovascular disease

Anna Rolleston (The Centre for Health) described MENZACS (Multi-Ethnic New Zealand study of Acute Coronary Care Syndromes) as the first foray into a true partnership bridging matauranga Māori and western science in heart health.
Professor Greg Jones (University of Otago) explained how analyses of DNA markers can uncover unknown exposures to environmental toxins, such as passive smoking, and improve the prediction of disease risk. This information could eventually enable more personalised risk assessment and would allow health issues to be followed up at an early stage.
Co-chair Associate Professor Peter Larsen (Otago University) summed up the session by recalling the excitement he felt when the first human genome was sequenced 21 years ago. For the promise of genomic technologies to be fully realized, genetic data will have to be held centrally, he said. And before this can happen, we need high levels of public trust, robust legal frameworks, and more investment in precision medicine research and infrastructure.
Developing precise and equitable cardiovascular disease risk prediction tools [38 min]
REPORT LAUNCH
Co-designing health research in Aotearoa New Zealand:
Lessons from the Healthier Lives National Science Challenge
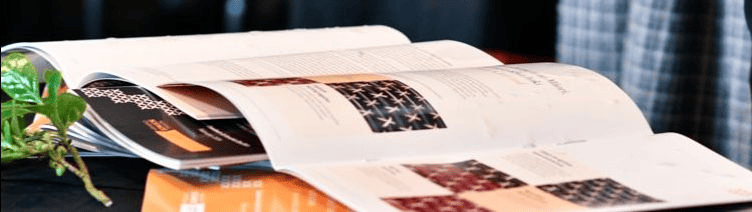
The Healthier Lives report Co-designing health research in Aotearoa New Zealand and accompanying Short Guide were officially launched at Kōrero Tahi 2024 in a blessing ceremony led by Toa Waaka, Rautaki Hononga Māori at the University of Otago Wellington.

Lead author Dr Debbie Goodwin (DBZ Consultancy) spoke about her Kaupapa Māori evaluation of Healthier Lives co-designed research projects, and the lessons learnt about how to co-design with integrity. Co-author Dr Amohia Boulton (Whakauae Research Services) explained the genesis of the reports in conversations around the Healthier Lives governance table and underlined the value of these new resources for researchers working with communities in Aotearoa New Zealand.
Co-designing health research in Aotearoa New Zealand [25 min]

Front: Toa Waaka, Justine Camp*, Helen Nicholson*, Libby Harrison*, Amohia Boulton*, Andrew Sporle*
[* Healthier Lives Governance Group and Kāhui Māori]
Co-designing health research in Aotearoa New Zealand – full report [PDF]
Co-designing health research in Aotearoa New Zealand – short guide [PDF]