Healthier Lives Newsletter May 2023
17 May 2023
In this issue:
- Congratulations to Associate Professor Dianne Sika-Paotonu
- Call for a National Food Strategy
- Updated food guidelines for the management of diabetes
- Replacing red and processed meat in our diet
- Implementation network – calling on researchers
- National nutrition survey awaited
- Upcoming events
Congratulations to A/Prof Dianne Sika-Paotonu

Healthier Lives warmly congratulates Associate Professor Dianne Sika-Paotonu on being awarded the Prime Minister’s 2022 Puiaki Whakapā Pūtaiao Science Communication Prize in recognition of her role as a leading voice during the Covid-19 pandemic explaining complex scientific information to the public.
We’re privileged to have A/Prof Sika-Paotonu as a member of the Healthier Lives Science Leadership Team and a co-Principal Investigator of the Healthier Lives Implementation Network.
Call for a National Food Strategy
An invitation to comment on international diabetes research findings of key importance to New Zealanders has prompted a call to action.
Healthier Lives researchers Andrew Reynolds and Jim Mann were recently invited to write a commentary on an article in Nature Medicine, one of the world’s leading health journals, which has highlighted the extent to which cases of type 2 diabetes are attributable to dietary factors.
Seven out of every ten cases of type 2 diabetes are associated with dietary factors. Some of the same dietary factors are also associated with frequently occurring cancers and coronary heart disease.
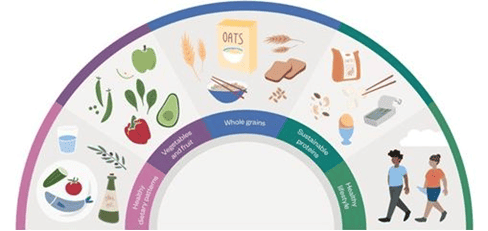
The study included data from 184 countries and showed that eating plenty of whole grains, vegetables, fruit, yoghurt, nuts, and seeds reduced the risk of developing type 2 diabetes. On the other hand, eating refined grains (e.g. white bread, white pasta and white rice), red meats, processed meats (e.g. salami and bacon), and drinking sugary beverages (including fruit juices) was associated with a higher risk of type 2 diabetes.
Other Healthier Lives research led by Cristina Cleghorn shows that an optimal diet for New Zealanders would not only offer protection against type 2 diabetes, heart disease and cancer but would also have a lower environmental impact in Aotearoa; the foods that benefit our health also produce lower greenhouse gas emissions.
In light of these findings, Prof Jim Mann has called on the New Zealand government to establish a Ministerial Taskforce to develop a national food strategy. Such a strategy would encompass the key role that food plays in our health, in our environment and in our economy. This would enable the coordinated large-scale government action needed to collectively tackle major issues facing Aotearoa New Zealand.
Read the commentary in Nature Medicine.
Read some of the national press coverage: RNZ article; New Zealand Doctor article.
Updated food guidelines for the management of diabetes

New Zealand researchers Andrew Reynolds and Jim Mann have made a significant contribution to newly updated European guidelines for the management of diabetes, published in the international journal Diabetologia. The guidelines were developed by The Diabetes and Nutrition Study Group of the European Association for the Study of Diabetes, a group established by Jim Mann almost 40 years ago.
These evidence-based recommendations for the nutritional management of diabetes were developed to inform discussions between health professionals and patients about managing diabetes and also to facilitate the prevention of type 2 diabetes.
The updated guidelines endorse the importance of high intakes of whole grains, vegetables, whole fruit, legumes, nuts, and seeds while minimising the consumption of red and processed meats, sugar-sweetened beverages and refined grains. They also focus on other forms of patient support, the environmental sustainability of foods, and the effects of ultra-processed food on health.
The potential to achieve remission of type 2 diabetes through dietitian-supported weight loss using meal replacement diets is included in the updated guidelines for the first time. This type of approach, developed through research in the UK and USA, will be rolled out to all parts of England by March 2024. A Healthier Lives study led by Kim Ma’ia’i, Justine Camp and Andrew Reynolds in conjunction with Te Kāika Health in South Dunedin is undertaking the first research trial to consider the cultural acceptability of this approach in Aotearoa New Zealand.
Read the guidelines in Diabetologia.
Replacing red and processed meat in our diet
Food production accounts for 26% of greenhouse gas emissions globally, with the production of red meat being the single largest food source of emissions. Excess consumption of red and processed meat is associated with the development of cardiovascular diseases, type 2 diabetes, and certain cancers such as colon cancer.
A recent research paper from Healthier Lives researchers Andrew Reynolds, Cristina Cleghorn, Cliona Ni Mhurchu and medical student Zi-Yi Kok investigated five novel scenarios that replaced some (or all) red and processed meat in the New Zealand diet with other protein-rich foods. The potential effect of these scenarios on the health of New Zealanders, equity in health outcomes for Māori, greenhouse gas emissions, costs to the health system, and grocery costs for individuals were investigated using modelling.
When compared with current red and processed meat intakes in New Zealand, all five replacement scenarios offered substantial gains. Replacing red meat with minimally-processed plant-based foods, such as legumes (e.g. kidney beans and lentils), showed the greatest potential benefits for the outcomes considered. While all New Zealanders would benefit from these scenarios, Māori health gains would be 1.6 to 2.3 times greater than that of non-Māori, which would help to narrow the current life expectancy gap in Aotearoa.
These findings confirm and extend current dietary advice to reduce red and processed meat intake (current Heart Foundation recommendations are to eat less than 50g per day), and to consume minimally processed rather than ultra-processed foods.
Achieving the benefits that this modelling shows is possible but will require Government action to introduce population-level initiatives that don’t rely on the agency of individuals, such as economic levers, food supply reformulation, and changes to the marketing of junk food. Such government-led initiatives are currently lacking, but are essential to protect the health of our communities.
This study is featured in an article by Niki Bezzant in the current issue of Listener magazine (May 20-26 2023).
Read the paper in eClinicalMedicine.

Healthier Lives Implementation Network – calling on researchers
The Healthier Lives Implementation Network aims to connect community health providers, researchers and people in the health system to help implement evidence-informed programmes and products that meet the health needs of Māori and Pacific communities.
Researchers invited to join Network
Researchers who would like to work in partnership with community health providers to help them adapt and implement health programmes or products developed through research are invited to join the Network. There may be an opportunity to create novel programmes with providers when existing programmes do not meet community needs. This invitation is warmly extended to all health researchers, not only those involved with Healthier Lives.
Sharing insights to improve implementation
The Implementation Network wants to understand researchers’ implementation experiences and challenges to facilitate more effective implementation in the future. We would like to hear from researchers about your experiences of implementation processes through this short survey which takes about 10 minutes to complete (research ethics information is on the first page): https://waikato.qualtrics.com/jfe/form/SV_5v7smrDcw24bptQ
Please consider sharing your insights via the survey and/or forwarding the survey link to others who might be able to contribute.
Contact
To express interest in joining the Network or ask questions about the survey, please contact Prof John Oetzel at .
For more information about the Network, visit its website.
National nutrition survey awaited
Researchers and health planners are eagerly awaiting an announcement about when the next national nutrition survey will take place. Until we have up-to-date data about what our population eats, we are flying blind when it comes to reducing the burden of diet-related disease in Aotearoa.
Regular surveys of our population’s dietary intake are critically important for measuring trends and informing the development of policy guidelines, regulations, and health programmes. For example, the 2008-09 national nutrition survey of adults resulted in recommendations to use iodised salt in bread and to fortify certain foods with folic acid, both of which are now mandated through legislation.
Huge differences in what New Zealand adults eat were found between the 2008-09 survey and the previous one in 1997. Now, more than 13 years on, it’s likely that even greater differences will be found when the next survey is undertaken. For tamariki, the changes may be even more profound. It is more than two decades since children were last surveyed in 2002.
In 2021, the Ministry of Health contracted a research group at the National Institute of Health Innovation (NIHI) to develop the methodology and tools for the next New Zealand nutrition survey. With 6 months of the 2-year project remaining, work is progressing well. The team, led by Healthier Lives Deputy Director Prof Cliona Ni Mhurchu, has developed, modified, and tested several useful tools for assessing NZ population diets, including a dietary habits questionnaire, updated food security questions, and an online semi-automated 24-hour dietary recall tool. When the next survey is scheduled, these new tools will enable comprehensive measurement of New Zealanders’ food and nutrient intakes and nutritional status.
Good health policy relies on health researchers and planners knowing what New Zealanders are eating. Obesity and poor nutrition are associated with premature death from coronary heart disease, type 2 diabetes and some cancers. Together, they have overtaken smoking as the number one health issue facing New Zealanders.
For more information, read the latest update from the New Zealand Nutrition Survey Development Team or register for this webinar:
Behind the Scenes: Developing Methods for a National Nutrition Survey
Thursday 13th July
10am – 11.30am
Register here
Upcoming events

The Edgar Diabetes and Obesity Research Centre (EDOR) is based in the Department of Medicine at the University of Otago. Healthier Lives works closely with EDOR on our shared goals to address the obesity and type 2 diabetes pandemics.
EDOR is celebrating 20 years as a Research Centre by holding an anniversary symposium at the Otago Museum’s Hutton Theatre on Friday 1st September. The keynote speaker for this event, Professor Mike Lean (University of Glasgow), will talk about his groundbreaking work on the remission of type 2 diabetes using the DiRECT clinical protocol, a dietitian-supported weight loss programme using meal replacement diets. This approach is being rolled out to all eligible people with type 2 diabetes in England by March 2024.
Healthier Lives is funding a New Zealand trial of the DiRECT protocol to determine the cultural acceptability of the programme for Māori and Pacific whānau.